Medicaid Redeterminations 2023
Among the many changes wrought by Covid-19 was declaration of a public health emergency (PHE) that ensured continuous enrollment in the Medicaid program for millions of low- and middle-income Americans. Under the PHE, states are required to keep people enrolled in Medicaid as a condition of receiving a temporary increase in the federal share of Medicaid costs. With usual verification requirements suspended during the PHE, many people who would normally have cycled out of the program are still covered, resulting in a caseload increase of 28% since the start of the pandemic.
Beginning April 1, 2023, states will be able to terminate Medicaid coverage for individuals who no longer qualify, requiring them to redetermine the eligibility status of an estimated 90 million enrollees. By some accounts, this transition, known as the “unwinding,” could lead to 18 million people losing health coverage. State Medicaid agencies are now mobilizing to plan their approaches and improve their overall redetermination and renewal processes.
The Imminent Risk
Even before the pandemic, Medicaid redeterminations were a source of coverage losses due to IT system delays and paperwork barriers. And even though the federal government requires states to start eligibility assessments using available data sources, some don’t use databases to full advantage. Alternatively, when renewal forms are mailed, complicated and confusing paperwork or frequent relocations can prevent people from responding on time or at all. The pandemic has only intensified these obstacles.
Furthermore, the Centers for Medicare and Medicaid Services (CMS) recently issued timelines for states to submit plans describing how they will approach the unwinding process. States failing to comply with these due dates and other conditions related to redeterminations could have their federal funding reduced.
Now’s the Time for Action
Large-scale Medicaid disenrollment when the PHE ends could have profound effects on the health and financial wellbeing of millions of people. The massive number of renewals and redeterminations is expected to strain the workforce and put existing processes to the test.
To avoid inappropriate terminations, CMS has recommended a number of PHE unwinding strategies. While each state’s specific plan will ultimately depend on their policies and IT capabilities, common to all is the need for a robust workforce to drive timely action. To this end, states should consider three strategies outlined below.
1. Assess Workload
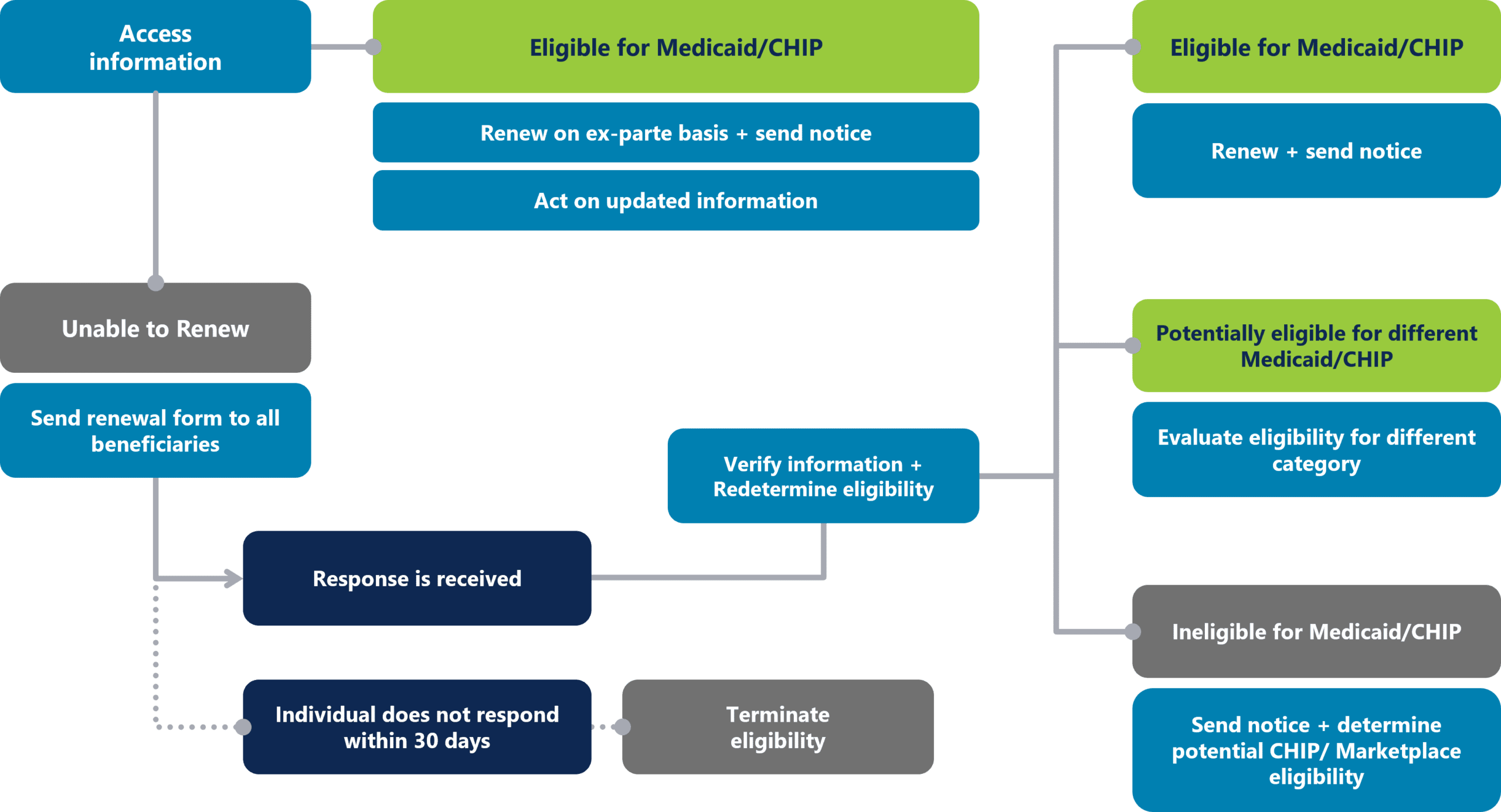
Accurate projections of the volume and type of work so that staffing needs can be determined are crucial to ensuring continuity of coverage. The graphic below illustrates the many components of the renewal and redetermination workflow.
To staff these functions for maximum performance, CMS advises using one or more of the following options:
-
- Redistribute existing workforce to ensure sufficient staffing across all affected units.
- Leverage contractors to support the current workforce where possible.
- Reassign workers from other state agencies.
With each approach, staff should receive ongoing training to understand current policies as well as temporary strategies for mitigating coverage loss.
2. Strengthen Automated Processes
Experts have observed that increasing the proportion of electronic redeterminations and renewals could be the most important single step states can take to prevent coverage losses.
Consequently, efforts to identify opportunities for automation, including ex parte renewals, no-touch case processing, and automated beneficiary communications like IVR messaging, are underway in many states.
States should also be able to accept applications and renewals online and over the phone, and if individuals are deemed ineligible, electronically forward their information to be evaluated for other coverage.
3. Adopt Workflow Efficiencies
When eligibility can’t be determined electronically, renewal forms sent to enrollees should be short and populated with information that’s already available. Communications should clearly explain the additional information needed, indicate where and when it should be sent, and offer resources for people who have questions.
Minimizing returned mail is also critical. This can be done through the use of existing data sources; outreach via email, texts, and telephone; and partnering with managed care plans, providers, and enrollment assisters. States should also identify specific roles that contractors can play in supporting unwinding efforts.
Leverage Healthcare BPO Partner
Healthcare advocates warn that problems such as outdated addresses for renewal notices and unreliable computer systems could hinder the ability of some of the most vulnerable Americans to afford care. If states implement the unwinding too quickly, incorrect contact information could proliferate, and call centers could be overwhelmed.
But these dire outcomes are preventable.
Third-party partners whose specialty is healthcare customer service, unlike other outsourcing partners, are uniquely positioned to improve the overall renewal process, strengthen communication, and leverage their experience to address beneficiaries’ needs while relieving the administrative burdens on state and local governments.
The BroadPath Advantage
- 15 Years of Experience
- 12 Medicaid Clients
- 700+ Medicaid Associates
